- Call Us: 7440777771
- |
- Mail: operation.eye@sbhhospital.com
Are you diabetic? Get yourself examined for Diabetic Retinopathy!
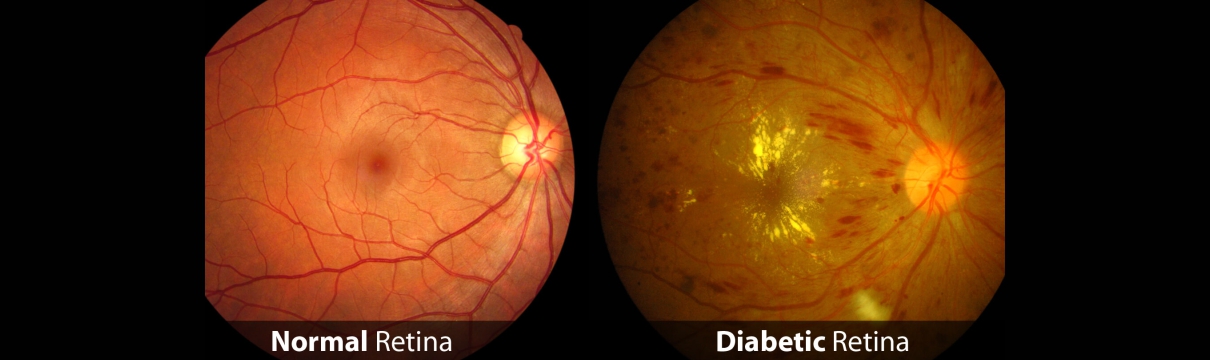
Diabetic retinopathy is referred to the damage caused to the retina precipitated by complications of diabetes mellitus.
The condition can progress to blindness if left untreated. Early blindness owing to diabetic retinopathy (DR) is generally preventable with routine checks and effective management of underlying diabetes.
Fast facts on diabetic retinopathy:
Diabetic retinopathy (DR) is blood vessel damage in the retina that happens because of diabetes.
It is one of the foremost causes of blindness.
Symptoms comprise difficulty seeing colors, blurred vision, floaters, and even complete loss of vision.
People with diabetes should have their vision examined at least once a year to rule out DR.
Despite the available retinal surgeries that can alleviate symptoms, but controlling diabetes and managing early symptoms are the most effective ways to prevent DR.
What is diabetic retinopathy?
Diabetic retinopathy is a complication of diabetes that can lead to total blindness if left untreated.
The retina is the membrane that covers the back of the eye and it is highly sensitive to light.
As it converts any light that hits the eye into signals that are interpreted by the brain, this process produces visual images, and it is how sight functions in the human eye.
Diabetic retinopathy damages the blood vessels within the retinal tissue, causing them to outflow fluid and distort vision.
There are two types of DR:
Non-proliferative diabetic retinopathy (NPDR): This is the milder form of diabetic retinopathy and is generally without any symptoms.
Proliferative diabetic retinopathy (PDR): PDR is known to be the most advanced stage of diabetic retinopathy and addresses the formation of new, anomalous blood vessels in the retina.
Globally, one-third of the estimated 285 million people with diabetes reflect signs of DR.
Symptoms
Diabetic retinopathy characteristically presents no symptoms during the early stages.
The condition is commonly at an advanced stage when symptoms become perceptible. On occasion, the sole noticeable symptom is an abrupt and complete loss of vision.
Signs and symptoms of diabetic retinopathy may include:
DR usually distresses both eyes. It is important to ascertain that the risk of vision loss is mitigated. The only way people with diabetes can avert DR is to regularly attend every eye examination as timely as scheduled by their doctor.
Complications
Possible complications commonly associated with diabetic retinopathy include the following:
Vitreous hemorrhage: Light is prevented from reaching the retina as the lately developed blood vessel seepages into the vitreous gel that fills the eye. Symptoms consist of loss of vision and sensitivity to light, or floaters in milder cases. This complication can resolve itself if the retina remains unharmed.
Detached retina: Scar tissue can wrench the retina away from the back of the eye. This generally causes the appearance of floating spots in the individual's field of vision, flashes of light, and severe vision loss. A detached retina signposts a significant risk of complete vision loss if left untreated.
Glaucoma: The normal flow of fluid in the eye may become congested as new blood vessels form. The obstruction causes a buildup of ocular pressure, or pressure in the eye, snowballing the risk of optic nerve damage and vision loss.
Causes and risk factors
Anybody with longstanding diabetes owns the risk of developing diabetic retinopathy. Nevertheless, there is a greater risk if the person:
Damage to the network of blood vessels that nourish the retina is the prime cause of diabetic retinopathy.
High glucose levels damage these vessels and limit the flow of blood to the retina. The problems with the blood vessels can be as insignificant as tiny bulges in the vessel wall that occasionally leak blood without distressing vision.
Nevertheless, in the advanced stages of the condition, these blood vessels may become completely choked. The eye then produces new, less stable blood vessels. The new vessels disrupt easily and outflow into the vitreous gel of the eye. The bleeding causes patchy and blurred patchy vision by further blocking the retina.
This bleeding, on occasion, causes scars that can disengage the retina and the eye, leading to a detached retina. As symptoms advance, a person with DR becomes more and more likely to experience complete vision loss.
Diagnosis
Diabetic retinopathy OCT
Diabetic retinopathy may be detected using an optical coherence tomography (OCT) scan.
Diabetic retinopathy usually starts without any noticeable change in vision. However, an ophthalmologist, or eye specialist, can detect the signs.
It is vital for people with diabetes to have an eye examination at least once or twice in a year, or when recommended by a physician.
The following methods are commonly employed to diagnose diabetic retinopathy:
Dilated eye exam
The doctor administers drops into the patient's eyes. These drops dilate the pupils and permit the doctor to view the inside of the eye in a more comprehensive way.
Photographs are taken of the interior of the eye. Through the eye examination, the doctor can detect the presence of:
These drops may sting, and the bright lights of the photographs can alarm the person receiving the test. In high-risk individuals, the eye drops may cause a rise in ocular pressure.
Fluorescein angiography
Drops are used to dilate the pupils, and a special dye known as fluorescein is injected into a vein in the patient's arm. Pictures are shot as the dye circulates through the eyes. The dye may drip into the retina or stain the blood vessels if the blood vessels are abnormal.
This test can determine which blood vessels are choked, dripping fluid, or broken down. Any laser treatments can then be precisely guided. For around 24 hours post the test, the skin may turn yellowish, and urine dark orange, as the dye exits the body.
Optical coherence tomography (OCT)
This non-invasive imaging scan offers high-resolution cross-sectional images of the retina, revealing its thickness. Post any treatments, scans may be used later to check how effective the treatment has been.
OCT is alike ultrasound testing but uses light rather than sound to produce images. The scan can also detect diseases of the optic nerve.
Treatment options
Treating DR depends on numerous factors, including the severity and type of DR, and how the person with DR has responded to previous treatments.
Individuals will require to work with their doctor to control diabetes. Good blood sugar control can significantly pace down the development of DR.
In most cases of PDR, the patient will need immediate surgical treatment. The following options are available:
Focal laser treatment, or photocoagulation
Vitrectomy
Surgery is not a remedy for diabetic retinopathy. Nevertheless, it may stop or slow the progression of symptoms. Diabetes is a long-term condition, and subsequent retinal damage and vision loss may still occur regardless of treatment.
Prevention
For the vast majority of people with diabetes, DR is an inevitable consequence.
Yet, patients with diabetes who effectively control their blood sugar levels will help to prevent the onset of a severe form of DR.
High blood pressure, or hypertension, is another causative factor. Patients with diabetes must control their blood pressure by:
Timely detection of symptoms increases the effectiveness of the treatment.
If you are diabetic or are suffering from any of the above-mentioned conditions, consult your doctor today!